There are three key parameters to consider when selecting and sizing a UV disinfection system:
To fully understand the principles of UV system selection, each parameter needs to be examined in more detail.
The nature and quality of the water to be disinfected are critical, and UV transmittance (UVT) is the most important of all the water quality parameters. UVT determines how easily UV-C light penetrates the water to get to the organism.
UVT is measured by taking a water sample in a quartz cuvette and passing UV light at 254nm through the sample. The percentage of UV light penetrating this sample is called the sample’s ‘UVT.’ Most typically, the cuvette used has a path length of 10mm, in which case the UVT reading is referred to as the ‘T10’ value. Other parameters such as biological oxygen demand (BOD), chemical oxygen demand (COD), turbidity, and total dissolved solids (TSS) may be an indication of the water quality and the UVT range to be expected, but only a direct measurement can be relied up as there is no correlation between these parameters and UVT.
If the water quality varies over time, a single spot sample can be unreliable, so samples should be taken over a representative period. Then, ensure that the UV system you select can deliver the required dose under those conditions.
Total Suspended solids (TSS) and total dissolved solids (TDS) or salinity are also important. TSS is particularly important because excessive TSS can result in a phenomenon known as ‘shielding’, whereby the pathogens are shielded from the UV-C light by particles suspended in the water. TDS/salinity is important because, at very high levels, attention must be paid to the construction materials of the UV system to avoid corrosion.
UV Inactivation is a very rapid process requiring only seconds, so UV treatment can offer a very compact and rapid treatment compared to alternative disinfection technologies.
But if the dose is defined as Intensity times residence time, then for any given reactor volume, the slower the flow rate of the water through it, the longer the UV exposure time and vice versa, so the water’s maximum and minimum flow rate are key performance parameters. This is why many UV systems now have the ability to adjust the power output of the lamps in relation to changes in water flow rate. By doing so, energy may be conserved when water flow rates are lower than peak flows.
It is important to establish the instantaneous flow rates when determining maximum and minimum flow rates, as this determines the instantaneous minimum and maximum UV exposure times. Daily and hourly flow rates are usually misleading in this respect, as they can mask important ‘peaks and troughs’ in the instantaneous flow rate, resulting in erratic calculations of the true UV exposure. In turbulent flow conditions, the residence time of organisms will vary, and hence, the dose received by each organism will be different. Any given reactor will have a characteristic Gaussian dose distribution, so beware of using average dose calculations in critical disinfection processes, as these are gross simplifications and can give a false sense of security.
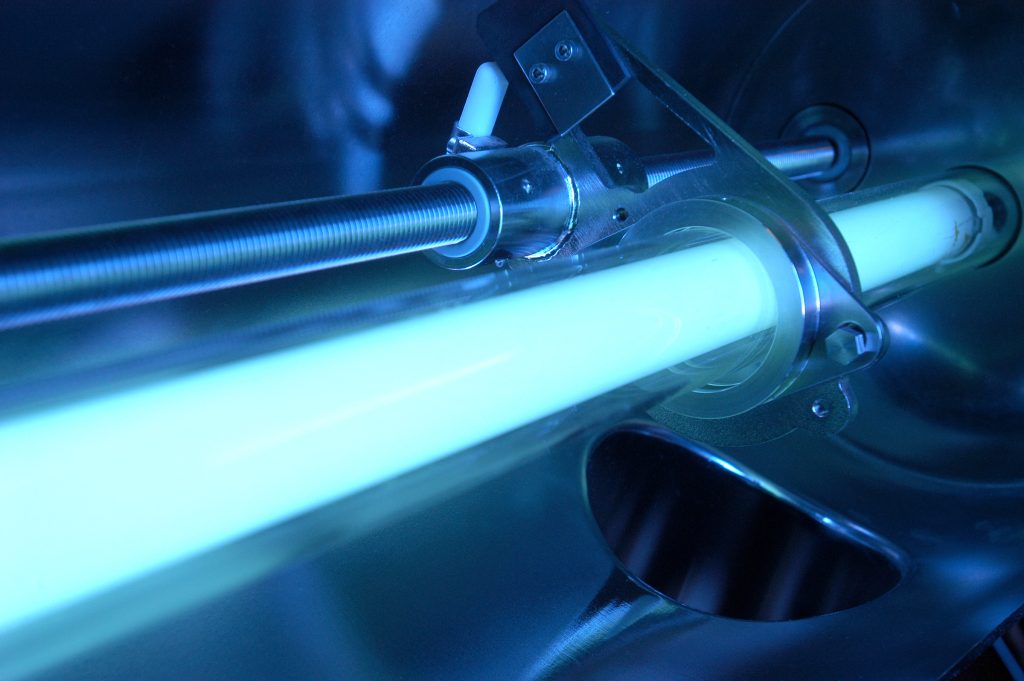
In the world of artificial lighting, Ultraviolet (UV) lamps stand as an intriguing and often overlooked category despite their widespread use across various industries. These lamps emit ultraviolet light and have unique properties and applications that make them indispensable in fields as diverse as healthcare, printing, water purification, and even forensics. This article will provide a detailed introduction to UV lamps, exploring their types, components, manufacturing process, applications, safety considerations, and their role in shaping the future of several industries.
UV lamps are specialized light sources designed to emit ultraviolet radiation. The ultraviolet spectrum consists of wavelengths shorter than visible light, and it can be divided into several categories, including UVA, UVB, and UVC, depending on the wavelength range. These lamps are engineered to produce UV radiation, and they find application in many fields due to their unique properties.
UV lamps come in various types, each with its characteristics and applications. Some of the most common types include:
A UV lamp is comprised of several key components that work together to produce ultraviolet light. Understanding these components is essential to grasp the lamp’s functionality:
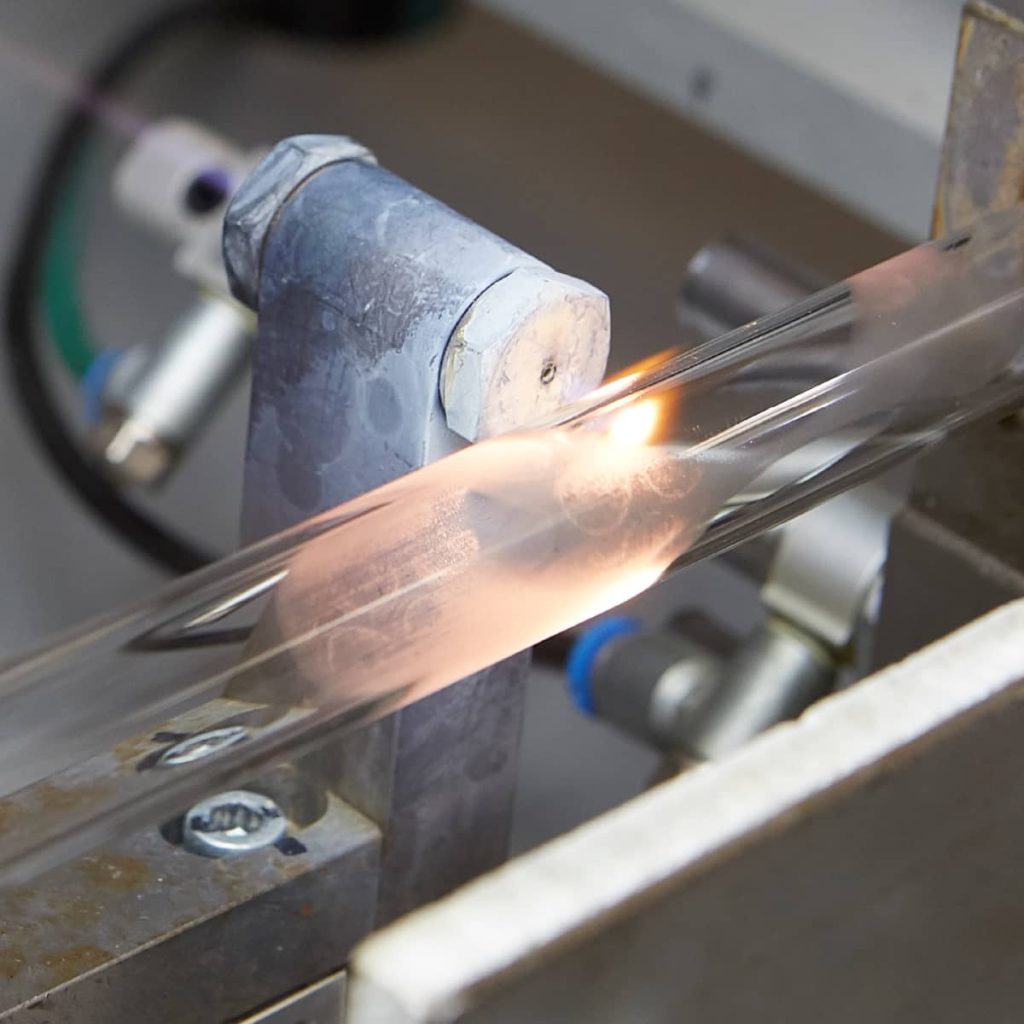
The production of UV lamps involves several intricate steps to ensure their quality and effectiveness:
Different pathogens have differing resistance to UV. Some are more susceptible than others and require different amounts of UV-C exposure for inactivation. There may even be a differing spectral response, i.e., the dose required can depend on the wavelength of UVC applied. In order to correctly size and select a UV system, it must be established which pathogen(s) are to be inactivated and what is there UV response characteristic.

What does inactivation truly mean? Does it mean every single pathogen that ever passes through the UV system will be inactivated? In reality, this is impossible; sterility is not economically achievable. Indeed, this is true regardless of what disinfection method is used, whether it is UV, chlorine, or anything else. What is possible is to reduce the pathogen count by a predictable amount. This predictable amount is called a ‘log’ reduction (as in logarithmic reduction). A 1 log reduction will reduce the pathogen of interest by 90% from the influent level. A 2-log reduction will see a 99% reduction, 3 3-log by 99.9%, and so on. Scientists have calculated the amount of UV exposure required to inactivate various pathogens by various log reductions. Examples appear in the table below.
A UV application requires a specified UV dose to achieve its required level of treatment. UV dose is the amount of UV energy per unit area on a surface. It is calculated as:
Dose = Intensity x Time (mJ/cm²)*
* The lamp power and Time of exposure to UV determine intensity. We will recommend the appropriate UV dose for each application, considering the lamp aging and fluid transmittance, the target organism, and required reduction. In the turbulent flow conditions of the UV reactor, not every particle of water or organism has the same residence time, which means that performance assessment is either a statistical calculation using Computer Fluid Dynamics (CFD) modeling or direct empirical measurement using a bioassay.
| TARGET PATHOGENS | LOG INACTIVATION | |||||||
| 0.5 | 1.0 | 1.5 | 2.0 | 2.5 | 3.0 | 3.5 | 4.0 | |
| CRYPTOSPORIDIUM | 1.6 | 2.5 | 3.9 | 5.8 | 8.5 | 12 | 15 | 22 |
| GIARDIA | 1.5 | 2.1 | 3.0 | 5.2 | 7.7 | 11 | 15 | 22 |
| VIRUS | 39 | 58 | 79 | 100 | 121 | 143 | 163 | 186 |
The amount of UV-C delivered to inactivate a pathogen has been called ‘UV exposure.’ The correct term for this exposure is ‘UV dose’ or ‘UV fluence.’ As the table above illustrates, the relationship between UV fluence and log reduction is described as a pathogen’s ‘Dose-Response Curve.’ As UV dose is the most common term for UV exposure, this will be used from here onwards.
It is important to note from the table above that the UV dose required to inactivate a given pathogen to a given log reduction is rarely linear. A common mistake is to take the UV dose required to achieve a 1-log inactivation and multiply it to calculate a higher log reduction. Although one very common pathogen, E. coli, has an almost linear dose-response curve, most are not.
For regulated applications such as drinking water, the answer is easy: you have a defined target pathogen and have to achieve a given log reduction, and a validation protocol is laid down.
In industrial applications, your choices are wider. Do you want:
These considerations will help you select a dose level, whether your UV needs validation or requires a hygienic design.
Share your treatment needs with us, and we will recommend a design philosophy. As a first approach, we suggest you consider a pathogen barrier at the beginning of your process to ensure that they do not populate your downstream equipment, and then use a hygiene maintenance philosophy to control secondary contamination after treatment and in distribution and storage. If your process is critical, we recommend a bioassayed or validated pathogen barrier as proof of performance. See our PQ systems.
Our hygienic designs will help maintain low bacterial counts when part of a hygienically designed system. i.e., a system continuously circulated at velocities > 1m / sec, is kept below 20C, has no dead legs, and is crevice-free and highly polished. Routine CIP will also be required to ensure that biofilms do not build up, but a good UV will extend the period between CIPs, reducing downtime and running costs.
Ultraviolet (UV) lamps have gained significant attention in recent years as a powerful tool for disinfection. They are employed in various settings, from healthcare facilities and public transportation to schools and households, to combat the spread of pathogens, including bacteria and viruses. While UV lamps offer an efficient means of disinfection, their use requires careful attention to safety. This article will delve into the world of UV lamp safety for disinfection, exploring the potential risks, protective measures, and regulatory guidelines to ensure their safe and effective operation.

UV disinfection is based on the principle that certain wavelengths of ultraviolet light, particularly UVC (254 nanometers), can damage the DNA and RNA of microorganisms, rendering them unable to replicate or function. This process effectively deactivates a wide range of pathogens, making UV lamps a valuable tool in infection control.
However, when used improperly, the same property that makes UV lamps effective—their ability to damage genetic material—also poses risks to human health and safety. Therefore, it is crucial to be aware of the potential hazards and follow best practices to ensure safe disinfection.
Skin and Eye Damage: Direct exposure to UVC radiation can cause skin burns and eye damage. It is essential to avoid looking at UV lamps and to shield exposed skin during operation.
Inadequate Disinfection: Insufficient UV exposure or improper lamp placement may result in incomplete disinfection, as not all surfaces or areas receive adequate UV radiation.
Ozone Production: Some UV lamps generate ozone as a byproduct, which can be harmful when inhaled in excessive amounts. The production of ozone should be minimized or controlled.
Chemical Contamination: Improper use of UV lamps can lead to contamination of surfaces or materials with hazardous chemicals, such as mercury, from UV-C lamps.
To mitigate the potential risks associated with UV lamp disinfection, various safety measures and best practices must be implemented:
Use Protective Gear: When operating UV lamps, use appropriate personal protective equipment (PPE), including UV-blocking eyewear, gloves, and clothing that covers exposed skin.
Occupancy Control: Ensure that no individuals are present in the room or area undergoing disinfection. UV lamps should only be operated in unoccupied spaces.
Proper Lamp Placement: Position UV lamps strategically to cover the area needing disinfection, considering reflective surfaces and shadowed areas.
Manufacturer Guidelines: Follow the manufacturer’s instructions for lamp operation, maintenance, and safety precautions. Each type of UV lamp may have specific recommendations.
Monitoring and Control: Implement monitoring and control systems to ensure that UV lamps operate as intended and that the disinfection process is effective.
Minimize Ozone Production: If UV lamps produce ozone, ensure the concentration remains within safe limits. Adequate ventilation may be required.
Regulatory Compliance: Be aware of and comply with local and national regulations and safety standards for UV disinfection. This includes proper labeling, handling, and disposal of UV lamps.
Training and Education: Provide adequate training to individuals responsible for operating UV lamps to ensure they know the risks and safety measures.
Many countries and regions have established regulatory guidelines to govern the safe use of UV lamps for disinfection. Compliance with these regulations is essential to protect the operators and those who may encounter the disinfected spaces.
For example, the Occupational Safety and Health Administration (OSHA) in the United States has specific guidelines regarding UV radiation exposure limits and using UV lamps for disinfection. These limits are designed to prevent harm to workers and ensure safe operations.
Organizations like the International Ultraviolet Association (IUVA) also provide resources and best practices to promote safe UV disinfection. IUVA emphasizes the importance of understanding the science behind UV disinfection and adhering to established safety guidelines.
It is imperative for institutions and individuals using UV lamps to familiarize themselves with local and international regulations and standards to ensure safe and effective disinfection practices.
UV lamp disinfection has found applications in a wide range of settings, each requiring specific safety considerations:
Healthcare Facilities: UV lamps disinfect patient rooms, operating theaters, and equipment. Strict safety protocols are followed to protect patients and healthcare workers.
Transportation: Public transportation systems, airports, and commercial vehicles use UV lamps for disinfection, requiring safety measures to prevent passenger exposure.
Schools and Educational Institutions: Disinfecting classrooms and common areas requires careful planning and scheduling to avoid exposure to students and staff.
Food and Beverage Industry: UV lamps are used for water disinfection in food processing, breweries, and wineries, necessitating strict safety and compliance with regulations.
Residential Use: UV lamps are increasingly used in homes to disinfect small spaces, necessitating awareness and adherence to safety guidelines among users.
Laboratories and Research Facilities: UV lamps are used in laboratories for disinfection purposes. Researchers and lab technicians must follow strict safety procedures.
The Role of UV Lamp Safety in the Fight Against Pathogens
UV lamp disinfection has proven to be a valuable tool in combating infectious diseases, especially when traditional cleaning methods are insufficient. However, safety must be a top priority, and operators and users are responsible for ensuring that UV lamp disinfection is conducted safely and effectively.
When employed with due diligence and strict adherence to safety measures and regulations, UV lamp disinfection can contribute significantly to preventing disease transmission and protecting public health. As technology advances and our understanding of UV disinfection deepens, we can harness its power while keeping health and well-being at the forefront of our efforts.